Plantar Fasciitis: Understanding Your Recurring Heel Pain
Heel pain can be more than a nuisance—it can slow you down, affect your work, and even make daily activities painful. One of the most common culprits behind chronic heel discomfort is plantar fasciitis, a condition that affects the thick band of tissue (the plantar fascia) connecting your heel to your toes. If you’ve experienced recurring heel pain, especially in the morning or after long periods of standing, it’s time to understand what plantar fasciitis is, why it happens, and how you can treat it effectively.
With the right combination of orthotics, shockwave therapy, and targeted rehabilitation exercises, you can regain pain-free steps and prevent future flare-ups.
What Is Plantar Fasciitis?
Plantar fasciitis occurs when the plantar fascia—a thick, fibrous band along the bottom of your foot—becomes inflamed. This tissue plays a crucial role in supporting your arch and absorbing the stress of walking or running. Over time, repeated strain can cause tiny tears, inflammation, and stiffness.
The pain is often described as sharp, stabbing, or burning, and many patients notice it most with the first steps in the morning or after long periods of sitting. While plantar fasciitis is common in runners, athletes, and people who spend long hours on their feet, it can affect anyone.
Common Symptoms of Plantar Fasciitis
Recognizing plantar fasciitis early can help prevent chronic issues. Typical symptoms include:
Sharp heel pain in the morning or after inactivity – Often called “first-step pain,” this is the hallmark symptom.
Pain after prolonged standing or walking – Especially on hard surfaces.
Stiffness in the arch of the foot – Your foot may feel tight and tender along the bottom.
Swelling or inflammation near the heel – Mild redness or warmth can sometimes accompany the discomfort.
Symptoms often start gradually, making them easy to ignore, but untreated plantar fasciitis can become chronic and harder to manage over time.
Causes and Risk Factors
Understanding the causes of plantar fasciitis can help you take preventive steps. Common factors include:
High-impact activities: Running, jumping, or sports that stress the heel can damage the plantar fascia.
Foot mechanics issues: Flat feet, high arches, or abnormal walking patterns can increase strain on the fascia.
Obesity or sudden weight gain: Extra weight puts additional stress on the heel and arch.
Age-related wear and tear: Plantar fasciitis is most common between ages 40–60.
Improper footwear: Shoes lacking support, cushioning, or proper fit can contribute to chronic stress.
It’s often a combination of factors rather than a single cause. Identifying your specific risk factors is key to both treatment and prevention.
Diagnosing Plantar Fasciitis
A proper diagnosis ensures you get the right treatment. Most cases are diagnosed based on:
Physical examination: Your doctor will check for tenderness along the heel and plantar fascia.
Medical history: Questions about your activity level, footwear, and previous injuries help pinpoint causes.
Imaging tests (if needed): X-rays or ultrasound can rule out other issues, such as fractures or bone spurs.
Early diagnosis allows for conservative treatments, which are often highly effective. Delaying evaluation can lead to chronic pain and more invasive interventions.
Treatment Options for Plantar Fasciitis
The good news: plantar fasciitis is treatable, and many patients find relief without surgery. Treatment focuses on reducing inflammation, relieving stress on the fascia, and promoting healing. Here’s how professional care can help:
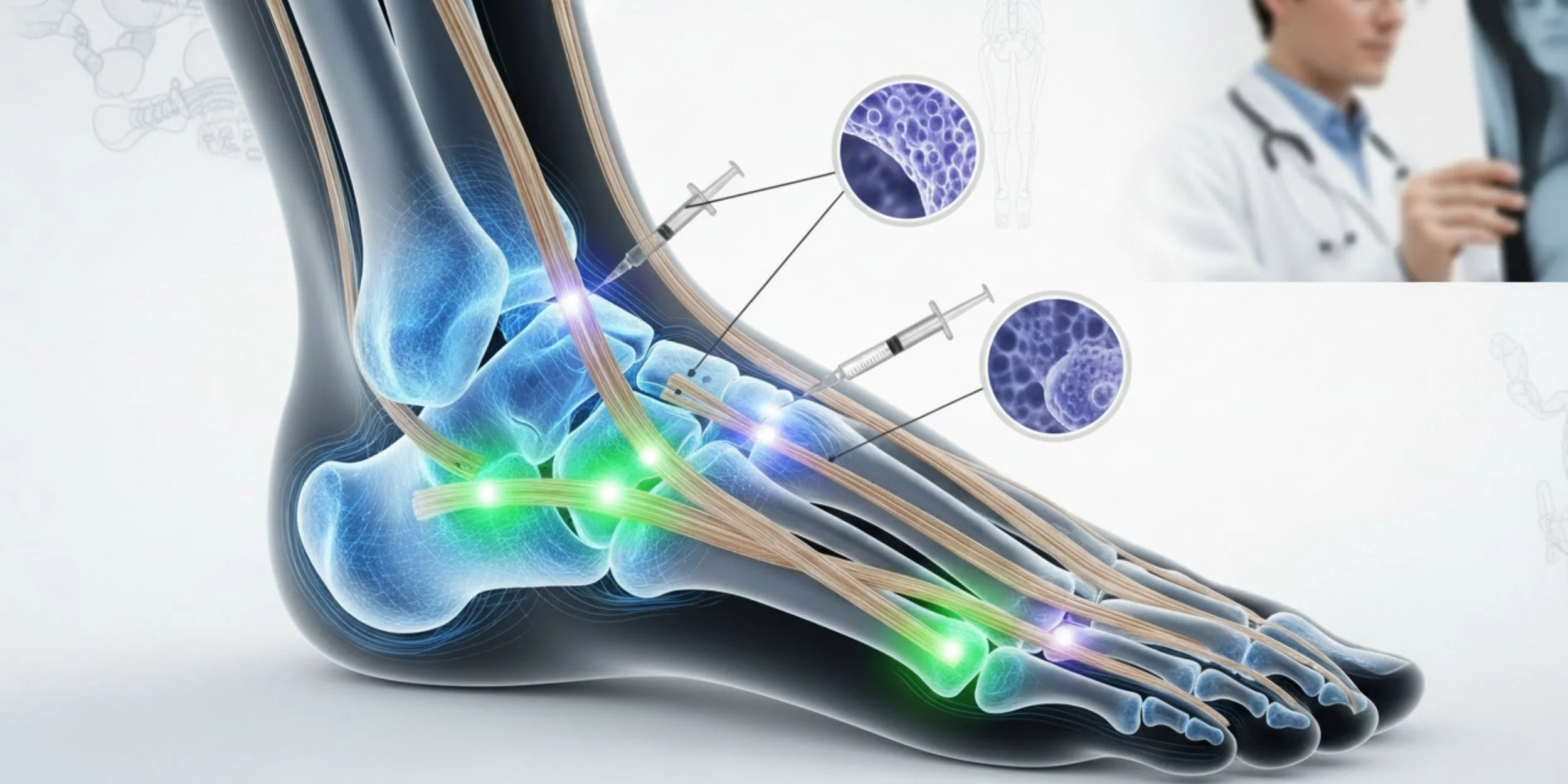
1. Custom Orthotics
Orthotics are specially designed shoe inserts that provide arch support, cushion the heel, and correct abnormal foot mechanics. By redistributing pressure, orthotics reduce strain on the plantar fascia, allowing it to heal and preventing future flare-ups. Many patients experience significant relief within weeks of consistent use.
2. Shockwave Therapy
For chronic or stubborn cases, extracorporeal shockwave therapy (ESWT) is a non-invasive option that stimulates tissue repair and improves blood flow to the affected area. It’s especially effective when pain persists despite orthotics and other conservative measures. Most patients tolerate the treatment well and can resume daily activities almost immediately.
3. Targeted Rehabilitation Exercises
Strengthening and stretching the foot, ankle, and calf muscles can alleviate heel pain and prevent recurrence. Physical therapy exercises focus on:
Stretching the plantar fascia and Achilles tendon
Strengthening the intrinsic muscles of the foot
Improving overall gait and foot mechanics
When combined with orthotics and professional guidance, rehab exercises provide a holistic approach that addresses both symptoms and root causes.
4. Anti-inflammatory Measures
Short-term options like NSAIDs (over-the-counter or prescribed), ice therapy, or corticosteroid injections can reduce pain and inflammation, but they don’t address the underlying mechanics of plantar fasciitis. They are most effective as part of a comprehensive plan.
Home Remedies and Lifestyle Changes
Alongside professional treatment, simple home care can make a difference:
Rest and ice: Apply ice to the heel for 15–20 minutes several times a day to reduce inflammation.
Proper footwear: Choose shoes with good arch support and cushioning. Avoid walking barefoot on hard surfaces.
Night splints: Wearing a splint at night gently stretches the plantar fascia and Achilles tendon while you sleep.
Activity modification: Reduce high-impact activities temporarily to allow the tissue to heal.
Consistency is key—combining home care with professional interventions accelerates recovery.
Exercises to Alleviate Heel Pain
Regular stretching and strengthening exercises help relieve pain and prevent future flare-ups. Some effective routines include:
Calf Stretch: Stand facing a wall, place one foot back, and gently lean forward while keeping the heel on the ground. Hold 20–30 seconds per leg, 3–5 times daily.
Plantar Fascia Stretch: Sit, cross your affected foot over the other knee, and gently pull your toes toward you. Hold for 15–30 seconds, repeat 3–5 times.
Towel Curls: Place a towel on the floor and use your toes to scrunch it toward you. Repeat 10–15 times per foot to strengthen arch muscles.
Marble Pickup: Use your toes to pick up marbles or small objects from the floor. Repeat for 2–3 minutes daily.
Performing these exercises consistently can improve flexibility, reduce tension, and speed healing.
Preventing Plantar Fasciitis Recurrence
Even after recovery, it’s important to take steps to prevent plantar fasciitis from returning:
Wear supportive shoes consistently, not just during workouts.
Maintain a healthy weight to reduce stress on your feet.
Gradually increase exercise intensity to avoid overloading the plantar fascia.
Incorporate regular stretching into your routine, especially for runners and active adults.
Prevention is always easier than managing chronic pain, so these habits are crucial for long-term foot health.
When to See a Doctor
While many cases improve with home care and conservative treatment, you should consult a healthcare professional if:
Pain persists beyond a few weeks despite self-care
Heel pain worsens or becomes severe
You notice swelling, redness, or numbness
Pain interferes with daily activities or exercise
Early professional intervention—like custom orthotics, shockwave therapy, and guided rehab—can significantly reduce recovery time and prevent long-term complications.
Conclusion and Key Takeaways
Plantar fasciitis is a common but manageable condition. With the right approach, including orthotics, shockwave therapy, and targeted rehabilitation, you can:
Reduce pain and inflammation
Correct underlying foot mechanics
Strengthen muscles to prevent recurrence
Resume daily activities comfortably
Ignoring recurring heel pain may lead to chronic discomfort or even additional foot problems. Taking action early ensures a faster, more effective recovery and keeps you moving without pain.
Take the First Step Toward Pain-Free Feet
If heel pain is limiting your life, don’t wait. Schedule a consultation today to explore personalized solutions, including custom orthotics, shockwave therapy, and rehab exercises tailored to your needs. Your journey to pain-free steps starts now.